Patient Information
Spine
Select from your area of interest below:
Currently viewing: Spine
When do you need a spinal implant?
Your orthopaedic surgeon will evaluate your situation carefully if you are experiencing pain, numbness, tingling or abnormalities as a result of a diseased or damaged spinal segments.
Common conditions in skeletally mature patients include:
- Arthrodesis required at any paired vertebral bodies in the cervical, thoracic, lumbar and/or sacral spine, as specified on the particular device’s label.
- Degenerative disc disease defined as back pain of discogenic origin with degeneration of the disc confirmed by history and radiographic studies.
- Spinal stenosis.
- Spinal deformities or curvatures.
- Spondylolisthesis.
- Trauma e.g. fracture or dislocation.
- Pseudoarthrosis.
- Previous failed fusion.
- Tumour.
- Can be used with osteobiological products such as OP1, BMP or similar.
In these cases, Signature Orthopaedics spinal implants can be employed to immobilize, stabilize or fuse a vertebral body.
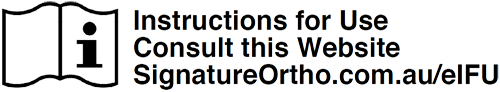
What is an ACDF surgery?
The Anterior Cervical Discectomy and Fusion (ACDF) surgery aims to relieve the pressure on the spinal cord, nerve roots and/or treat an unhealthy disc in the cervical spine.
Through a small incision, the surgeon will have direct access to the cervical spine from the front, where the removal of themdamaged disc can take place, followed by the placement of interbody fusion implant.
To secure the vertebrae in place during the fusion of bone, spinal implants such as a standalone implant, with built-in fixation (i.e. screws) or plate with screws may be used. Over time, the vertebrae is expected to grow together through fusion. This may take from a few months, to a few years to completely fuse depending on patient factors.
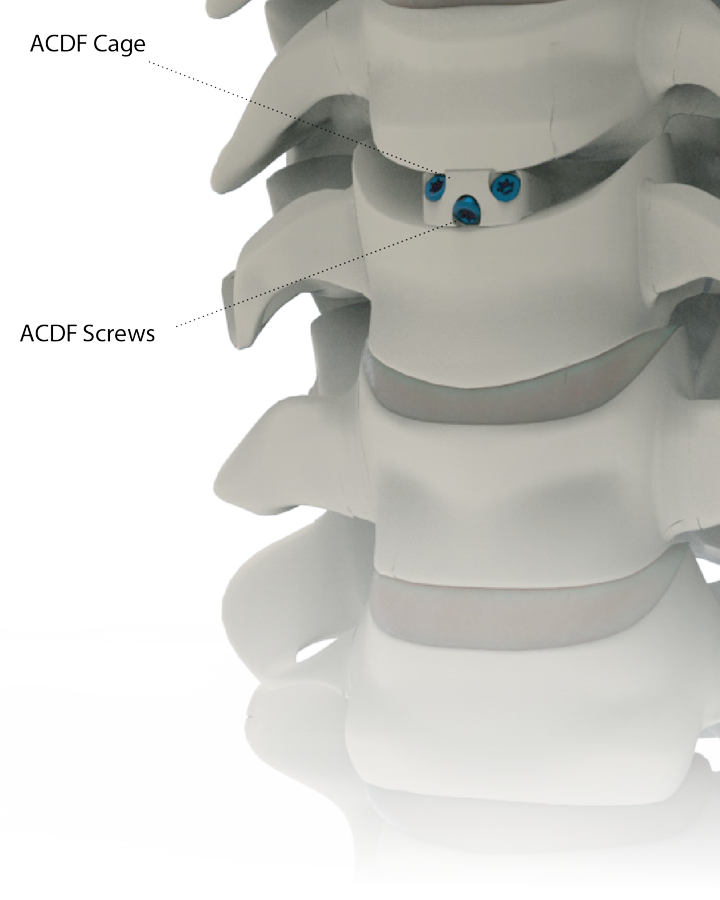

What is an ALIF surgery?
The Anterior Lumber Interbody Fusion (ALIF) surgery aims to relieve the pressure on the spinal cord, nerve roots and/or treat an unhealthy disc in the lumbar spine.
Through a small incision, the surgeon will have direct access to the lumbar spine from the front, where the removal of the damaged disc can take place, followed by the placement of interbody fusion implant.
To secure the vertebrae in place during fusion of bone, spinal implants such as a standalone implant with built-in fixation (i.e. screws) or plate with screws may be used. Over time, the vertebrae is expected to grow together through fusion. This may take from a few months, to a few years to completely fuse, depending on patient factors.
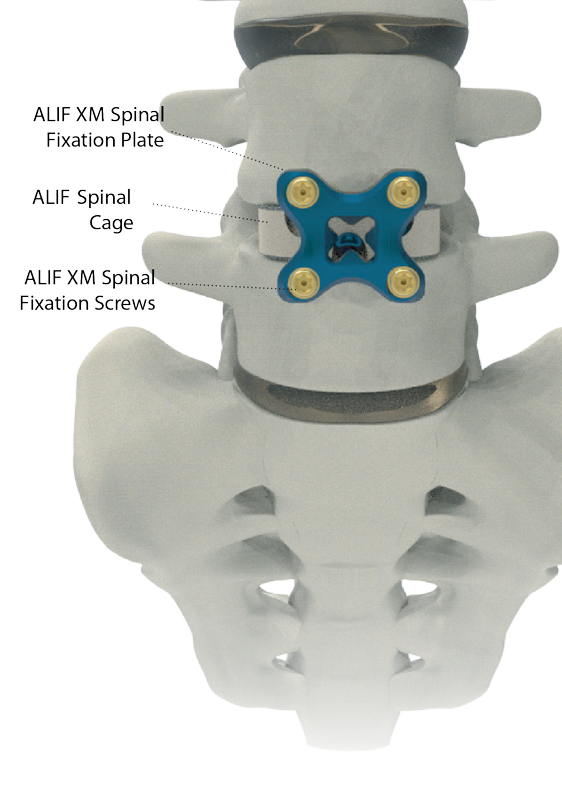

What is an PLIF surgery?
The Posterior Lumbar Interbody Fusion (PLIF) surgery aims to relieve the pressure on the spinal cord, nerve roots and/or treat an unhealthy disc in the lumbar spine.
Through a small incision, the surgeon will have direct access to the lumbar spine from the back, where the removal of the damaged disc can take place followed by the placement of an interbody fusion implant.
To secure the vertebrae in place during fusion of bone, spinal implants such as an interbody spacer is inserted into the disc space. Screws and rods are inserted on the left and right sides of the vertebrae to hold the vertebrae in place. Over time, the vertebrae is expected to grow together through fusion. This may take from a few months, to a few years to completely fuse, depending on patient factors.

What is a minimally invasive surgery?
A Minimally Invasive Surgery (MIS) involves the use of small incisions along the spine where the surgeon is able to separate the muscles surrounding the spine instead of cutting through them.
As surgery is personalized to patient factors and symptoms, your orthopaedic surgeon will discuss if minimally invasive surgery is right for you.

How long will my implants last?
The device is not intended to support in-vivo loading indefinitely. Over time, the vertebral bone is expected to grow together over time through fusion. This may take from a few months, to a few years to completely fuse, depending on patient factors.

Which implant is right for me?
Although implant surgery is extremely successful in most cases, some patients will still experience pain and stiffness. Your physician will evaluate your particular situation carefully before making any decision regarding which implant is most appropriate for you, and discuss all complications and risks with you prior to surgery.
Signature Orthopaedics’ spinal implant is only intended for use with approved devices and accessories. The selection of an implant of the correct size, shape, and type of bone fixation is extremely important to maximise the potential for a successful, long-term outcome for you.

Adverse Events and Risks
The following are specific adverse effects which should be understood by the surgeon and explained to the patient.These warnings do not include all adverse effects that may occur in surgery.
- Nonunion (pseudarthrosis).
- Bending or fracture of implant.
- Early or late loosening of the implant.
- Metal sensitivity, or allergic reaction to the implant.
- Early or late infection.
- Decrease in bone density due to stress shielding.
- Pain, discomfort, or abnormal sensations.
- Various nerve and vascular damage.
- Bursitis.
- Paralysis.
- Dural tears experienced during surgery could result in the need for further surgery, a chronic CSF leak or fistula and possible meningitis.
- Damage to lymphatic vessels and/or lymphatic fluid.
- Spinal cord impingement or damage.
- Cessation of growth of the operated portion of the bone.
- Fracture of bony structures, or penetration of the implant into the bone.
- Bone formation around and through the implant making removal difficult.
- Post operative change in spinal curvature, loss of correction, height and/or reduction.
- Degenerative changes or instability in segments adjacent to fused vertebral levels.

Will I return to everyday activities?
The degree to which you can perform day to day movements is based on your range of motion as shown below. A normal knee would have a range of motion up to 0 to 135 degrees of flexion (bending) and 120 to 0 degrees of extension (straightening).
The decision on your post-operative activity level is dependent on your surgeon’s recommendations and guidelines as well as your compliance with recommended post-operative therapy.